Translate this page into:
The role of cone-beam computed tomography in evaluation of an extensive radicular cyst of the maxilla
*Corresponding author: Nishat Hussaini, Department of Conservative Dentistry and Endodontics, Oxford Dental College, Bengaluru, Karnataka, India. nish.huss@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Althaf S, Hussaini N, Srirekha A, Santhosh L. The role of cone-beam computed tomography in evaluation of an extensive radicular cyst of the maxilla. J Restor Dent Endod 2021;1(1):30-3.
Abstract
Radicular cyst is the second most common odontogenic cyst. Most of these lesions involve the apex of offending tooth and appear as well-defined radiolucencies. When asymptomatic, a cyst can acquire a large size, even extending into anatomic cavities. The present case reports an extensive radicular cyst extending into the maxillary sinus that could have been easily mistaken for just a displaced tooth. Conventional radiographs show two-dimensional images of three-dimensional objects. Cone-beam computed tomography provides undistorted three-dimensional information of hard tissues, gives adequate spatial resolution, and recently seen as an expansion in diagnosis and management of periapical lesions. Prompt diagnosis and treatment of radicular cyst were successful with endodontic treatment and surgical management.
Keywords
Cone-beam computed tomography
Enucleation
Odontogenic cyst
Radicular cyst
Root canal therapy
INTRODUCTION
Radicular cyst can be referred by multiple names such as dental cyst, periapical cyst, apical periodontal cyst, or root-end cyst.[1] It is the most common cyst of the jaws, with frequency of about 7–54% in the permanent dentition.[2] It is more frequent in maxillary (60%) than mandibular teeth, especially in incisor-canine region.[3] It has the highest in the third and fourth decade of life and mostly seen in males.[4]
Radicular cyst is inflammatory in origin, which originates from epithelial cell rests of Malassez in the periodontal ligament.[3] Radicular cysts are direct sequel to chronic apical periodontitis but not every chronic lesion develops into a cyst. They develop as a progression of untreated dental caries with pulp necrosis and periapical infection around the apices of the teeth involved, but in relation to accessory root canals, they can also be found on the lateral aspects of the roots.[5] Many of the studies have shown a weak association between the size of radiolucencies and histological findings of radicular cysts.[6] The treatment options for radicular cyst can be conventional nonsurgical root canal therapy (RCT) when lesion is localized or surgical treatment such as enucleation, marsupialization,[7] or decompression when the lesion is large.
This case report presents the cone-beam computed tomography (CBCT) analysis and treatment plan of an extensive radicular cyst. The conventional radiographs show a two-dimensional image of the three-dimensional object and its surrounding structures. CBCT provides three-dimensional images of the object from sagittal, coronal, and axial directions to overcome image defects, such as overlap and deformation.[2] Hence, this article reports a rare case of an extensive radicular cyst associated with maxillary right central incisor with the use of CBCT in diagnosing and management.
CASE REPORT
A 22-year-old female patient reported to the department with a chief complaint of irregularly arranged upper anteriors with a history of trauma 10 years back. There was a displacement of teeth which compromised her esthetic appearance [Figure 1a]. On clinical examination, Ellis Class II fracture in #11 and Ellis class I fracture in relation to #22 was observed. Teeth were not mobile and no tenderness on percussion was seen. Pulp sensibility test showed no response in relation to 11 and 12. The adjacent teeth elicited normal response. Careful inspection and palpation of buccal vestibule did not reveal any expansion of bone or draining sinus tract. Lymph nodes were non-palpable. Intraoral periapical radiograph, orthopantomogram (OPG), and occlusal radiograph [Figure 1b] revealed unilocular radiolucency extending from maxillary right central incisor to maxillary right first molar (11–16) and into the maxillary sinus with well defined, well corticated radio-opaque borders. Routine laboratory investigations were within normal limits.
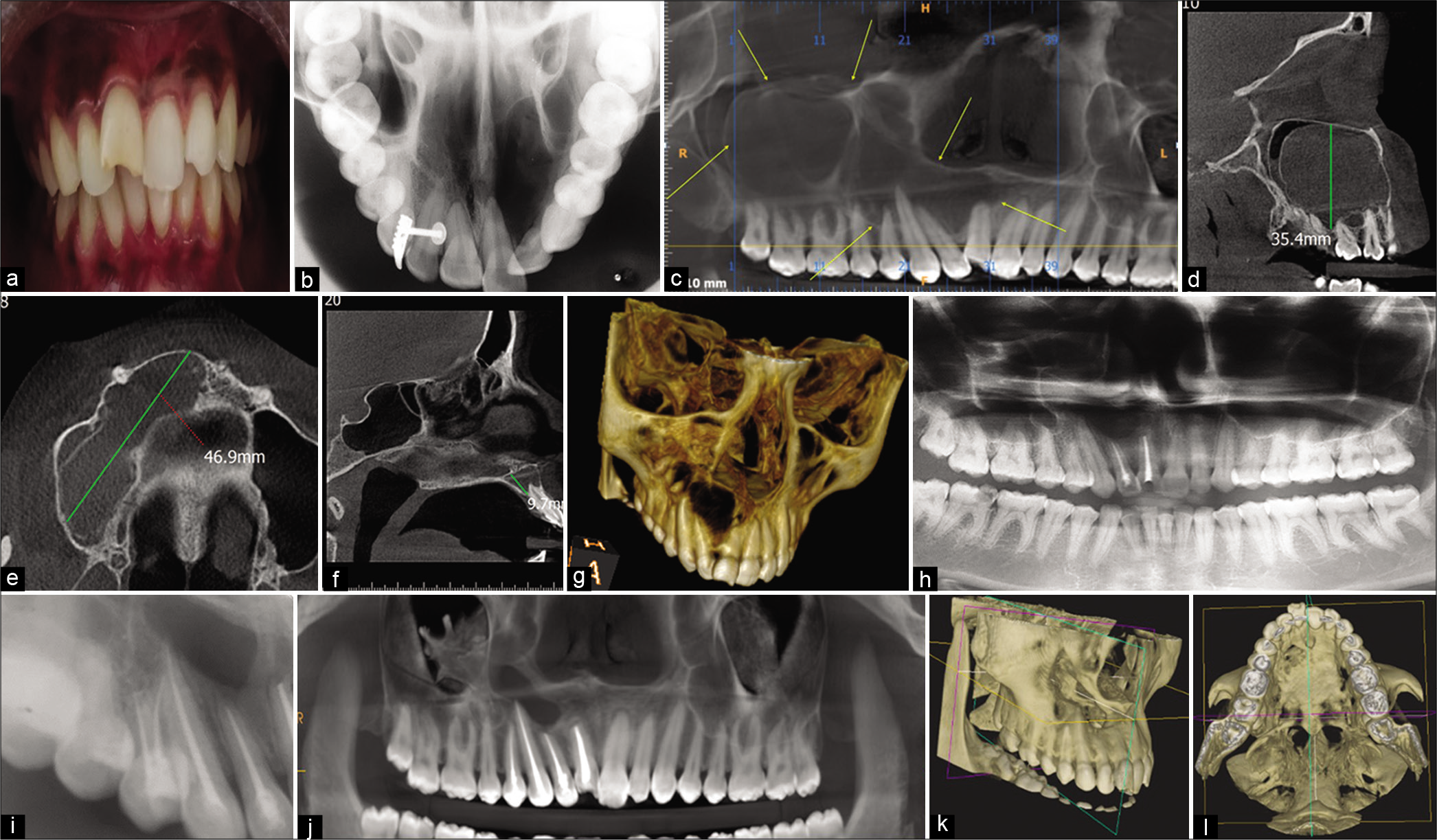
- (a) Pre-operative clinical picture showing displaced teeth, (b) Occlusal radiograph showing the lesion, (c) CBCT image showing the extent of the lesion marked with arrows, (d) Oblique section, (e) Axial section, (f) Axial section, (g) 3D reconstructed view of the extent of the lesion, (h) Post-surgical follow-up OPG, (i) Non-vital 13, 14, and RC treated, (j) Two-year follow-up CBCT, (k) 3D reconstructed views of the lesion demonstrating healing. Note the reduced size, (l) 3D reconstructed views of the lesion demonstrating healing. Note the reduced size.
CBCT revealed osteolytic lesion with sclerotic margin in the periapical region of 11. The lesion was well-defined, unilocular, uniformly radiolucent involving the right maxillary dentoalveolar region, extending from mesial aspect of 11 to peri-apical region of 11, 12, 13, and ballooning into the right maxillary sinus with approximate size as marked in the sections measuring about 46.9 mm × 35.4 mm × 9.7 mm in dimension [Figure 1c-g]. The lesion almost entirely occupied the right maxillary sinus approximating the floor of the orbital floor and lateral borders of the nasal fossa. Lesion was roughly oval in shape and had corticated borders. Epicenter of the lesion appeared to be the peri-apical region of 11. Displacement of the roots of 11, 12, and 13 was noted. No clear evidence of external root resorption was noted with respect to the associated teeth except for mild apical blunting of the roots with respect to 11, 12, and 13. Expansion, thinning, and perforation of labial, palatal cortical plates, and also the floor and lateral borders of the nasal fossa were noted.
Lesion closely approximated the incisive canal. Based on radiographic examination and CBCT evaluation, a definitive diagnosis of cyst was made, but the final call for type of cyst was left to the histopathological report. Before the incisional biopsy, aspiration was done and it yielded yellow fluid, further strengthening the suspicion of radicular cyst. Treatment plan comprised of RCT for 11, 12, and cyst enucleation. Enucleation of the cyst was performed under local anesthesia and as the cystic cavity was infected and was very large so bone grafting was not considered and the defect was left for secondary healing. Apicoectomy was performed and root end was burnished using a hot burnisher. Histopathological examination revealed non-keratinized stratified squamous epithelium cystic lining. The connective tissue capsule was fibrovascular with dense inflammatory filtrate composed of lymphocytes and plasma cells. Few areas of extravasated red blood cells were also seen. The histological features confirmed the diagnosis of radicular cyst.
Outcome and follow-up
Post-surgical follow-up after 15 days showed prompt healing of the surgical site. At 6 months follow-up, there was no increase in size of the lesion and OPG revealed a new bone formation at the site of cystic lesion [Figure 1h]. On the other hand, pulp sensibility showed no pulpal response in relation to 13 and 14 for which endodontic treatment was initiated [Figure 1i].
Two-year follow-up
On the follow-up visit, in comparison with the previous CBCT records, the lesion showed a reduced size and increased bone fill in the area of the lesion [Figure1j-l]. The area internal to the defect exhibited radiodensity equivalent to soft tissue. Breach in the jaw boundaries was still noted at the area of defect, buccally, palatally, and at the floor of the nasal fossa. As the patient was keen on improving her esthetics, orthodontic treatment was planned, but it was ruled out as there was not enough bone formation around that area. Conservative management was suggested to improve esthetics to a certain extent.
DISCUSSION
The term “cyst” is a Greek word, “Kystis,” which means “sac or bladder.”[8] Cyst is an epithelium-lined pathological cavity with a centrifugal, expansive mode of growth.[9] Radicular cysts originate after trauma or dental caries leading to pulpal necrosis.[10] In the present case, the patient gave a history of trauma, which could be the probable etiology. The progression of the lesion depends not only on the status of immunity of the individual, local predisposing factors but also on last and the most important factor duration of the disease and this could be a possible reason for the huge increase in size over a period of time.[11] Most of the radicular cysts are usually asymptomatic and are accidentally detected on plain OPG while investigating for other diseases. Clinically, radicular cyst may present as a swelling which is hard in consistency and shows buccal or palatal cortical expansion. There may be areas of decortication confirmed clinically by yielding on palpation.[3] The present case was associated with no such enlargement which is not common; however, CBCT showed expansion, thinning, and perforation of labial and palatal cortical plates. In the present case, there is a possibility that as the enlarging cyst gained entry into the maxillary sinus, it restricted the bony expansion. The expanding cyst can cause mobility and displacement of teeth, and in the present case, the main complaint was displacement of anterior tooth. The cyst may cause mild root resorption and can even cause nerve compression.[5] Massive dental cysts may sometimes extend away from the original epicenter[12] into the maxillary sinus and sometimes present as a large radicular cyst and the present case was similar.
Radiographically, the radicular cyst appears as round or pear-shaped unilocular radiolucency at the apex of a non-vital tooth as in the present case but was an extensive lesion. Other odontogenic cysts such as dentigerous cysts, odontogenic keratocysts, and odontogenic tumors such as mural ameloblastoma, Pindborg tumor, and odontogenic fibroma may share similar radiological features. Hence, histopathological evaluation is necessary to diagnose these giant lesions. In extensive lesions, radiographs alone may not be sufficient to show the full extent of the lesions, and advanced imaging is needed.[5,13] CBCT provides a 3D image that allows complete visualization of an area in question, in axial plane, the sagittal, and coronal planes and it also adds depth of field to conventional radiographs.[14] Thus, in this case, use of CBCT preoperatively helped in assessing the extent of the cyst and to plan the surgery better than with conventional radiographs because of its ability of 3D reconstructions in the craniofacial region. Postoperatively, CBCT benefited the patient in evaluating the outcome of healing and prognosis.
The recommended treatment option available for radicular cyst is the conventional endodontic approach combined with decompression or surgical enucleation of a cyst.[7] The treatment of these cysts is still under discussion and many professionals opt for a conservative treatment by means of endodontic technique. Enucleation of large cysts in the jaws is an invasive method that may lead to complications such as damage of the adjacent teeth or anatomic structures, but less invasive surgical techniques for treating large radicular cysts have been developed such as endoscopically assisted enucleation.[15] The present case was an extensive cyst; hence, one-step conventional surgical enucleation was performed, as this is a preferred treatment option in treating massive lesions. Although care was taken during the surgical procedure, the vitality of the adjacent teeth was violated and therefore RCT was performed for 13 and 14.
Healing of the periapical area after 2-year follow-up also is not complete, which could be due to the large area of destruction. At present, the patient is asymptomatic and has been kept under observation for future recall.
CONCLUSION
The current concept in the management of periapical cysts is the non-operative mode of treatment. However, surgical management might be necessary for successful treatment, depending on the size and extent of the lesion. The clinical case reported in this article was successfully managed by endodontic therapy followed by surgical intervention. Integration of digital technology into endodontic practice has opened up new opportunities for diagnosis, treatment planning (pre-surgical assessment), and for follow-up.
Acknowledgment
We would like to thank the department of oral and maxillofacial surgery and the department of oral pathology and histology for their support.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Shafer's Textbook of Oral Pathology (6th ed). New Delhi: Elsevier; 2009. p. :487-90.
- [Google Scholar]
- Radicular cyst associated with a primary first molar: A case report. J Dent. 2011;8:213-7.
- [Google Scholar]
- CBCT assessment of healing of a large radicular cyst treated with enucleation followed by PRF and osseograft placement: A case report. Saudi J Oral Dent Res. 2017;2:72-5.
- [Google Scholar]
- Clinical and radiological features of a large radicular cyst involving the entire maxillary sinus. MUSBED. 2012;2:31-6.
- [Google Scholar]
- Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med. 2006;35:500-7.
- [CrossRef] [PubMed] [Google Scholar]
- Management of infected radicular cyst by surgical decompression. J Conserv Dent. 2010;13:159-61.
- [CrossRef] [PubMed] [Google Scholar]
- New perspectives on radicular cysts: Do they heal? Int Endod J. 1998;31:155-60.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 2007;33:908-16.
- [CrossRef] [PubMed] [Google Scholar]
- Role of inflammation in developmental odontogenic pathosis. J Oral Maxillofac Pathol. 2016;1:164.
- [CrossRef] [PubMed] [Google Scholar]
- Giant radicular cyst of the maxilla. BMJ Case Rep. 2014;2014:bcr2014203678.
- [CrossRef] [PubMed] [Google Scholar]
- The use of cone beam CT in cranio-maxillofacial surgery. Int Congr Ser. 2005;1281:1200-4.
- [CrossRef] [Google Scholar]
- Use of dentomaxillofacial cone beam computed tomography in dentistry. World J Radiol. 2015;6:128-30.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopically assisted enucleation of a large mandibular periapical cyst. Stomatologija. 2011;13:128-31.
- [Google Scholar]