Translate this page into:
The effect of Erbium-doped Yttrium Aluminum Garnet laser irradiation on push-out bond strength of endodontic sealers with root canal dentin: An in vitro evaluation of push-out bond strength and failure modes

*Corresponding author: Nilima Salim Isani, Department of Conservative Dentistry and Endodontics, Krishnadevaraya College of Dental Sciences and Hospital, International Airport Road, Hunasamaranahalli, Yelahanka, Bengaluru - 562 157, Karnataka, India. nilimaisani94@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Reddy JS, Jayalakshmi KB, Sujatha I, Nadig P, Isani NS, Elizabeth D. The effect of Erbium-doped Yttrium Aluminum Garnet laser irradiation on push-out bond strength of endodontic sealers with root canal dentin: An in vitro evaluation of push-out bond strength and failure modes. J Restor Dent Endod 2021;1(1):2-8.
Abstract
Objectives:
The aim of this study was to evaluate and compare the push-out bond strength of bioceramic sealer and resin-based sealer on Erbium-doped Yttrium Aluminum Garnet (Er:YAG) treated root canals.
Material and Methods:
Sixty single-rooted teeth were collected, decoronated apical to the cementoenamel junction, maintaining the minimum root length of 14 mm. Samples were instrumented with WaveOne Gold primary file and divided into two experimental groups (n = 30), based on laser irradiation: Group I: No laser and Group II: Er:YAG laser irradiated. Groups I and II were again divided into two subgroups “a” (AH Plus) and “b” (mineral trioxide aggregate [MTA] Fillapex) with 15 samples in each group. As per the grouping, sealers were coated onto the canal walls and obturated. After 24 h of storage in 100% humidity at 37°C, all the samples were sectioned transversely and push-out test was performed using universal testing machine. Stereomicroscope was used to determine the mode of failure. A one-way analysis of variance was employed to compare the mean POBS. Kolmogorov–Smirnov and Shapiro–Wilk parametric tests were done to check the normality. The Games-Howell multiple post hoc test was used for pairwise comparison of the groups at a 95% confidence level.
Results:
Both AH Plus and MTA Fillapex exhibited higher bond strength in the laser-treated canals. AH plus exhibited superior bond strength compared to MTA Fillapex in both laser and non-laser-treated groups (P < 0.05). AH Plus groups have predominantly presented cohesive failure whereas MTA Fillapex presented mixed failures.
Conclusion:
Irradiation with Er:YAG laser in the root canal before obturation improves the bond strength significantly. The adhesive properties of MTA Fillapex are comparable to that of AH Plus.
Keywords
Erbium-doped Yttrium Aluminum Garnet laser
AH plus
Mineral trioxide aggregate Fillapex
Push-out bond strength
Bioceramics
INTRODUCTION
A three-dimensionally obturated root canal system prevents percolation and microleakage of periapical exudates into the root canal space. It prevents reinfection and creates a favorable environment for healing to take place.[1] As gutta-percha does not bond to root canal wall, a wide array of sealers has been tested for obtaining a fluid tight seal in canal system.[2,3]
The bond strength of root canal sealers to dentin is crucial in providing the integrity of the seal at both static and dynamic conditions. In static situations, the adhesion eliminates spaces that allow the penetration of fluids into the sealer-dentin interface. However, in dynamic circumstances, occlusal forces may flex the tooth and dislodge the obturating material, this can be prevented by an adequate adhesion between the sealer, gutta-percha, and dentinal wall.[4,5]
Effective removal of the smear layer before obturation is of vital importance to achieve better bond strength and adaptability of root canal sealer to the canal walls. Several agents such as citric acid and EDTA solution have been tested for smear layer removal.[5] Lately, the advent of laser irradiation to promote root canal disinfection is gaining popularity. Erbium-doped Yttrium Aluminum Garnet (Er:YAG) laser is proposed to be effective in removing smear layer from canal walls and possibly more effectively than EDTA and citric acid.[6]
AH Plus (Dentsply DeTrey, Konstanz, Germany) is a commonly used epoxy resin-based sealer having excellent sealing properties and considered as a gold standard against which all new sealers are being compared.[6] Unremitting researches have introduced many contemporary sealers with superior physical, chemical, and enhanced antibacterial properties.[7] At present, bioceramics as sealer are gathering exceptional attention due to its ability to form hydroxyapatite and eventually create a bond between dentin and the filling material. Furthermore, the hydrophilic nature of this material is one of the proposed reasons for improvised adaptation. Mineral trioxide aggregate (MTA) Fillapex (Angelus, Londrina PR, Brazil) is a new biocompatible paste – paste MTA-based root canal sealer with a high sealing capacity. Besides, it is proposed to have bactericidal and cementum regeneration properties.[8]
Lasers, particularly hard tissue lasers, block the dentinal tubules by melting the dentinal surfaces. On the contrary, lasers with a wavelength range of 2700–3000 Nm (Er, Cr:YSGG, and Er:YAG lasers) have optimal interaction with water and hydroxyapatite, and therefore, the laser energy is highly absorbed by dental structures causing surface ablation.[9] Despite the desirable properties of the bioceramic sealers and high-intensity laser irradiation, it is less understood about their synergistic effect to improve the root canal seal and bond strength and, therefore, might enhance the success of root canal treatment.
Hence, the aim of this study was evaluate the push-out bond strength (POBS) of MTA Fillapex and AH Plus sealers in Er:YAG laser-treated root canals.
MATERIAL AND METHODS
Sample collection
Sixty intact single-rooted human permanent teeth were selected for the study. Samples were cleaned and stored in isotonic saline until further use.
Sample processing
The coronal portions of the teeth were sectioned with diamond coated disc (Horico) apical to the cementoenamel junction to standardize the root length to 14 mm, and the samples were stored at 37°C in 100% humidity until further use.
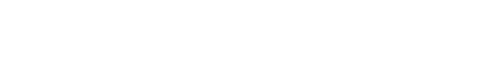
The biomechanical preparation was carried out using #10, #15, and #20 K-files (Dentsply Maillefer, Ballaigues, Switzerland) followed by WaveOne Gold primary file (Dentsply Maillefer, Ballaigues, Switzerland) up to the working length. About 17% EDTA (Meta Biomed) was used for lubrication and sequential irrigation was done with 5% sodium hypochlorite (DentPro). Deionized distilled water was used as the final irrigant. The samples were divided into two groups, Group I and Group II of 30 samples each. Group I samples did not receive laser irradiation. Canals of Group II were irradiated with Er:YAG laser (Fotona d.d. Stegne 7 ErIII, Slovenia, Fotona laser tip – Xpulse 600/14 cylindrical, conical). Groups I and II were further divided into subgroups “a” and “b” of 15 samples each. Subgroup “a” received AH Plus (Dentsply) and subgroup “b” received MTA Fillapex (Angelus) as sealer materials [Figure 1].
- Schematic representation of the grouping of samples.
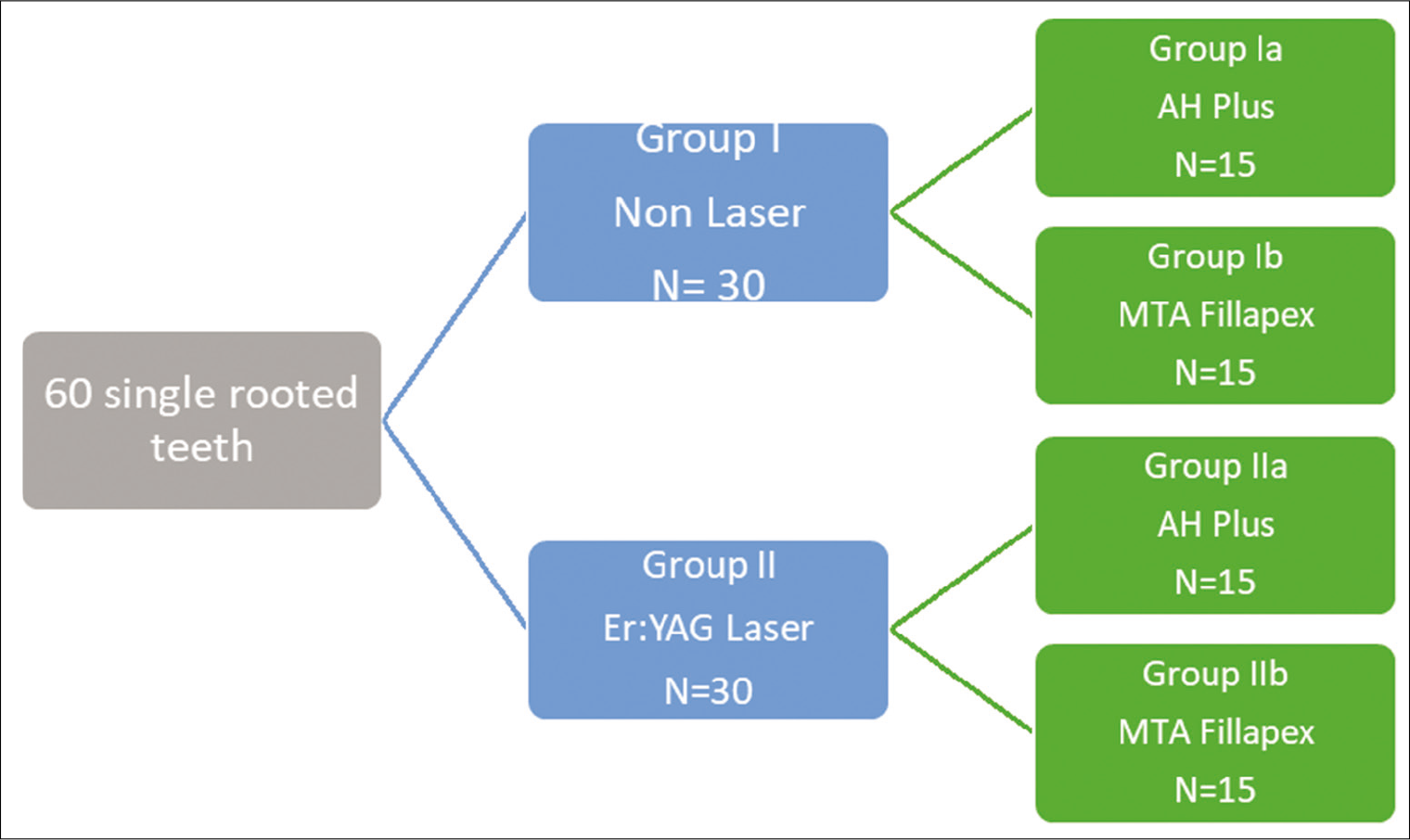
Laser irradiation was done using Er:YAG laser (Fotona d.d. Stegne 7 ErIII, Slovenia) at 20 Hz frequency, 125 mJ energy, 30 s application time, and 2.50 W power, underwater, and air coolants [Figure 2]. All root canals were irrigated with 5 ml of saline solution and carefully dried with WaveOne Gold primary paper points (Dentsply Maillefer, Ballaigues, Switzerland).
- Erbium-doped Yttrium Aluminum Garnet laser irradiation.
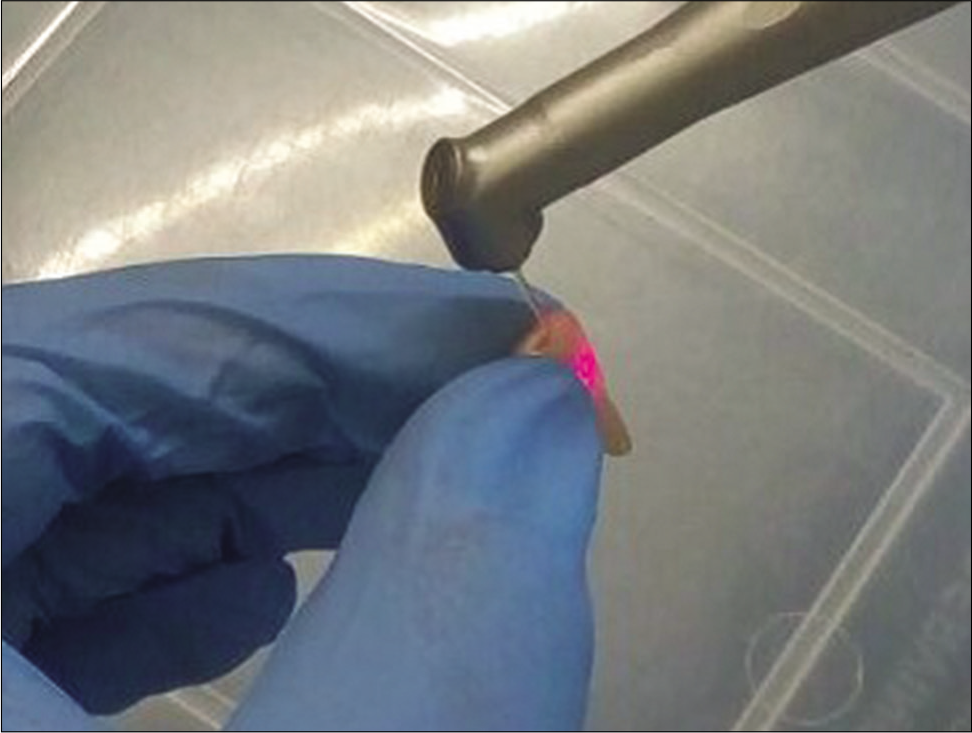
As per the grouping, the sealers were coated onto the canal walls using Lentulo spirals and the canals were obturated using WaveOne Gold primary gutta-percha points (single cone technique) (Dentsply Sirona, Ballaigues, Switzerland). After 24 h of storage in 100% humidity at 37°C, all samples were sectioned transversally at 2 mm and 4 mm distances, measured coronoapically to obtain a disc of the 2 mm thickness [Figure 3].
- Transverse sectioning of the specimen.
Push-out test was performed at 1 mm/min crosshead speed using a universal testing machine (Instron 4411, Instron Inc., Canton, MA, USA) having the tip diameter of 0.5 mm [Figure 4].[10] The maximum load at failure (Fmax) was recorded in N, and the bonding surface (A) in mm2 was calculated using the equation:
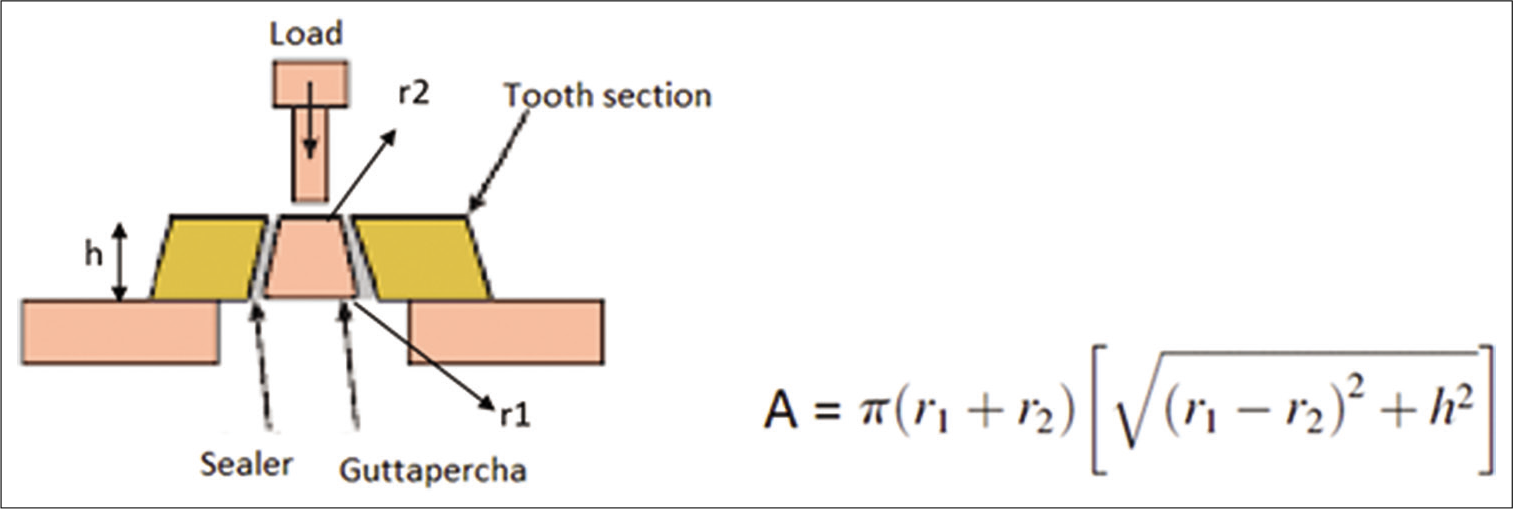
- Equation for calculating bonding surface (A) in mm2.
Where, π is the constant 3.14, r1 is the coronal radius, r2 is the apical radius, and h is the slice thickness in mm. POBS was calculated using the following equation
Push-out bond strength (MPa) = maximum load (N)/Bonding surface (mm2)
Statistical analysis was performed using collected data.
Failure mode analysis
The failure mode was analyzed under a stereomicroscope at ×40. Each specimen was identified according to the failure mode and was classified as an adhesive (failure at the sealer-dentin or the sealer-core material interface), cohesive (failure within sealer or dentin), or mixed (failure in both the sealer and dentin) failures.
Statistical analysis
Results were statistically analyzed using SPSS/PC software version 22 (IBM; Chicago; IL, USA). A one-way analysis of variance (ANOVA) was employed to compare the mean POBS. Kolmogorov–Smirnov and Shapiro–Wilk parametric tests were done to check the normality. The Games-Howell multiple post hoc test was used for pairwise comparison of the groups at a 95% confidence level.
RESULTS
In the current study, mean POBS scores of different groups are shown in Table 1, AH Plus sealer used in LASER irradiated canals showed significantly higher POBS (6.92 MPa), compared to the other groups.
| Groups | n | Minimum | Maximum | Mean | SD |
|---|---|---|---|---|---|
| Group Ia | 15 | 4.05 | 6.43 | 5.54 | 0.79 |
| Group Ib | 15 | 3.42 | 6.99 | 4.99 | 1.29 |
| Groups IIa | 15 | 5.45 | 7.97 | 6.93 | 0.90 |
| Group IIb | 15 | 4.55 | 7.84 | 6.07 | 1.08 |
n: Study sample number, Group Ia: No Laser+AH Plus, Group Ib: No Laser+MTA Fillapex, Group IIa: Laser+AH Plus, Group IIb: Laser+MTA Fillapex, Mpa: Megapascal, SD: Standard deviation
Mean POBS was higher in LASER irradiated groups when compared to non-LASER irradiated groups (4.99 and 5.54, respectively). Further, there was no significant difference between Group IIb (non-laser + MTA Fillapex) and any other group.
Mean POBS values were ranked as follows; Group IIa > Group IIb > Group Ia > Group Ib. ANOVA showed statistically significant differences among the tested groups (P < 0.05).
The distribution details of the data are shown in Table 2. Table 3 shows comparisons among the groups using one-way ANOVA Welch test. A significant difference (P < 0.05) was observed among the groups.
| Kolmogorov–Smirnov | Shapiro–Wilk | |||||||
|---|---|---|---|---|---|---|---|---|
| Statistic | df | Sig. | Statistic | df | Sig. | |||
| Group Ia | 0.21 | 15 | 0.06 | 0.88 | 15 | 0.05 | ||
| Group Ib | 0.22 | 15 | 0.04 | 0.87 | 15 | 0.03 | ||
| Group IIa | 0.16 | 15 | 0.20* | 0.91 | 15 | 0.13 | ||
| Group IIb | 0.19 | 15 | 0.18 | 0.93 | 15 | 0.31 | ||
*The mean difference is significant at the 0.05 level, Group Ia: No Laser+AH Plus, Group Ib: No Laser+MTA Fillapex, Group IIa: Laser+AH Plus, Group IIb: Laser+MTA Fillapex
| n | Mean (MPa) | Standard deviation | Standard error | 95% confidence interval for mean | Minimum | Maximum | P value | ||
|---|---|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||||
| Group Ia | 15 | 5.54 | 0.79 | 0.20 | 5.10 | 5.90 | 4.05 | 6.43 | <0.001 |
| Group Ib | 15 | 4.99 | 1.29 | 0.33 | 4.27 | 5.70 | 3.42 | 6.99 | |
| Group IIa | 15 | 6.93 | 0.90 | 0.23 | 6.43 | 7.42 | 5.45 | 7.97 | |
| Group IIb | 15 | 6.07 | 1.08 | 0.28 | 5.47 | 6.67 | 4.55 | 7.84 | |
| Total | 60 | 5.88 | 1.24 | 0.16 | 5.56 | 6.20 | 3.42 | 7.97 | |
n: Study sample number, Group Ia: No Laser+AH Plus, Group Ib: No Laser+MTA Fillapex, Group IIa: Laser+AH Plus, Group IIb: Laser+MTA Fillapex, Mpa: Megapascal, ANOVA: Analysis of variance
Multiple intergroup comparisons using Games-Howell post hoc test [Table 4] shows that laser-treated AH Plus groups show significant superiority (P < 0.05) in mean POBS over non-laser-treated AH Plus and MTA Fillapex groups. However, there is no significant difference between laser-treated AH Plus and laser-treated MTA Fillapex groups (P > 0.05). Furthermore, the non-significant difference was observed between AH Plus and MTA Fillapex in non-laser-treated groups (P > 0.05).
| (I) Groups | (J)Groups | Mean difference (I-J) | Standard error | Sig. | 95% confidence interval | |
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| Ia | Ib | 0.55 | 0.39 | 0.50 | −0.53 | 1.63 |
| IIb | −0.53 | 0.34 | 0.43 | −1.48 | 0.42 | |
| IIa | −1.39* | 0.31 | *0.001 | −2.23 | −0.55 | |
| Ib | Ia | −0.55 | 0.39 | 0.50 | −1.63 | 0.53 |
| IIb | −1.08 | 0.43 | 0.08 | −2.27 | 0.10 | |
| IIa | −1.94* | 0.40 | *0.00 | −3.05 | −0.83 | |
| IIa | Ib | 1.94180* | 0.40 | *0.001 | 0.83 | 3.06 |
| Ia | 1.39028* | 0.31 | *0.001 | 0.55 | 2.23 | |
| IIb | 0.86051 | 0.36 | 0.11 | −0.13 | 1.85 | |
| IIb | Ib | 1.08129 | 0.43 | 0.08 | −0.10 | 2.27 |
| Ia | 0.52977 | 0.34 | 0.43 | −0.42 | 1.48 | |
| IIa | −0.86051 | 0.36 | 0.11 | −1.85 | 0.12 | |
*The mean difference is significant at the 0.05 level, N: Study sample number, Group Ia: No Laser+AH Plus, Group Ib: No Laser+MTA Fillapex, Group IIa: Laser+AH Plus, Group IIb: Laser+MTA Fillapex
Results of the mode of failure indicate that most of the samples showed cohesive and mixed failures. The failure patterns for AH Plus sealer were predominantly cohesive and for MTA Fillapex were a mixed pattern.
DISCUSSION
As a consequence of biomechanical preparation, smear layer forms over the instrumented dentinal walls. This layer obstructs the penetration of sealer tags into the dentinal tubules and thereby decreases adhesion by micromechanical forces.[11-13] Although several demineralizing solutions have been tested to remove the smear layer, the complete desired accomplishment is still questionable. Furthermore, these acidic solutions may demineralize the intertubular dentine around tubular openings, which is trivial.[14,15]
According to available evidence, LASERS are effective in removing the smear layer.[14,16,17] Er-YAG has been proposed to be efficient in the removal of the smear layer from root canals.[14] Takeda et al. have evaluated the dentine permeability after treatment with Er:YAG laser. They concluded that there is an increase in smear layer removal and dentine permeability with Er:YAG laser.[14,16] These findings are ratified by a histological and scanning electron microscopic study by Kesler et al. (2002).[18] Hence, in the current study, Er:YAG laser was used to remove the smear layer from the root canals.
The POBS test is a mechanical test in which load is applied longitudinally to the long axis of the root until the material is dislodged; this establishes the bond strength or resistance to dislodgement. The push-out test has been commonly employed test to evaluate the dislodgement resistance on sectioned specimens of canal filled roots using a universal testing machine.[19,20] To simulate the dynamic dislodgement forces between root canal filling material and dentinal walls in the laboratory, POBS was employed in this study.[21]
The results of the present in vitro study showed that Group-II, that is, laser irradiated groups showed better POBS than Group-I where canals were without laser treatment. The probable reason could be that the laser irradiation produced melted and sealed tubules accompanied by evaporation of the organic matrix and could result in reduction of fluid permeability and thereby improving the adhesion of sealer to the canal walls.[22] Furthermore, the effective removal of smear layer followed by the opening of dentinal tubules and increased surface irregularities, which further increases the flow of sealer.[14,23] Improvised bond strength in laser-treated samples was also observed in a study by Ozkocak et al. (2015).[24]
The AH Plus sealer in both laser irradiated and non-laser irradiated groups in intergroup comparison showed higher POBS than the MTA Fillapex sealer. The reason could be related to the epoxy resin-based sealers having excellent physical properties such as longer setting time, low solubility, high-flow rate, thixotropicity (Miletic, 1999), low volumetric polymerization shrinkage, and good interfacial adaptation.[25]
Intragroup comparison of Group-I between “a” and “b” showed lower POBS of Group-Ib having MTA Fillapex as sealer, the reason quoted could be that MTA Fillapex includes MTA as one of the ingredients. The release of calcium and hydroxyl ions from the set sealer will result in the formation of appetites as the material comes in contact with phosphate-containing fluids which gets deposited with in the collagen fibrils, promoting mineral nucleation of dentine, which is seen as the formation of an interfacial layer with tags like structure, hence, the low bond strength could be because of low adhesion capacity of these tag-like structures.[26] Second MTA Fillapex, a self-cure cement containing calcium in its composition has low tensile cohesive strength which could have resulted in lesser POBS.[27]
In the current study, there is no statistical difference between the subgroups “a” and “b” in both the groups. MTA Fillapex has shown comparable POBS with that of AH Plus. These results are in accordance with the study done by Assmann et al. (2012), where MTA Fillapex has shown a non-significant difference in bond strength compared to AH Plus. The probable reason might be because of composition, shear rate, particle size, temperature, and mixing time will agitate the flow ability of sealers.[28,29] Contrarily, Sonmez et al. (2013) and Gupta et al. (2013) had proposed significant superiority of AH Plus over MTA-based sealer. The proposed reason behind the superiority of AH Plus is inherent physical properties such as longer setting time, low solubility, high-flow rate, thixotropicity, low volumetric polymerization shrinkage, and good interfacial adaptation.[30-32]
Based on the study results, it can be concluded that the POBS of root canal sealer is influenced by properties of the sealer and various dentine surface treatments. Removal of smear layer increases the POBS to root dentine as it favors better adaptation of the endodontic sealer.
CONCLUSION
Within the limitations of this study, it can be concluded that the application of Er:YAG laser improves the bond strength of both AH Plus and MTA Fillapex sealers.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Bioactive glasses in the management of dentine hypersensitivity: A review. Dent Health. 2017;3
- [CrossRef] [Google Scholar]
- Three-dimensional obturation of the root canal using injection-molded, thermoplasticized dental gutta-percha. J Endod. 1977;3:168-74.
- [CrossRef] [Google Scholar]
- Sealer penetration into dentinal tubules in the presence or absence of smear layer: A confocal laser scanning microscopic study. J Endod. 2014;40:1627-31.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of bond strength of different endodontic sealers to root dentin: An in vitro push-out test. J Conserv Dent. 2016;19:461-4.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of dentine pretreatment on the adhesion of root-canal sealers. Int Endod J. 2002;35:859-66.
- [CrossRef] [PubMed] [Google Scholar]
- Evolution of root canal sealers: An insight story. Eur J Gen Dent. 2013;2:199-218.
- [CrossRef] [Google Scholar]
- A comparative assessment of the antibacterial activity of root canal sealers on 2 Actinomyces species: An in vitro study. Adv Clin Exp Med. 2019;28:243-8.
- [CrossRef] [PubMed] [Google Scholar]
- Bioceramic-based root canal sealers: A review. Int J Biomater. 2016;2016:9753210.
- [CrossRef] [PubMed] [Google Scholar]
- Stimulatory effects of CO2 laser, Er: YAG laser and Ga-AlAs laser on exposed dentinal tubule orifices. J Clin Biochem Nutr. 2008;42:138-43.
- [CrossRef] [PubMed] [Google Scholar]
- Push-out bond strength of different tricalcium silicate-based filling materials to root dentin. Braz Oral Res. 2018;32:e18.
- [CrossRef] [PubMed] [Google Scholar]
- A preliminary scanning electron microscopic study of root canals after endodontic procedures. J Endod. 1975;1:238-42.
- [CrossRef] [Google Scholar]
- Influence of smear layer on depth of penetration of three endodontic sealers: An SEM study. Endod Dent Traumatol. 1998;14:191-5.
- [CrossRef] [PubMed] [Google Scholar]
- Sealer penetration into dentinal tubules in the presence or absence of smear layer: A confocal laser scanning microscopic study. J Endod. 2014;40:1627-31.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study of the removal of smear layer by three endodontic irrigants and two types of laser. Int Endod J. 1999;32:32-9.
- [CrossRef] [PubMed] [Google Scholar]
- Use of acid cleanser in endodontic therapy. J Am Dent Assoc. 1975;90:148-51.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of dentin root canal permeability after instrumentation and Er: YAG laser application. Lasers Surg Med. 2000;26:277-81.
- [CrossRef] [Google Scholar]
- In vitro evaluation of smear layer removal by Er: YAG laser application with five different fiber optic tip withdrawal techniques In: Lasers in Dentistry, International Society for Optics and Photonics. 2003. p. :188-95.
- [CrossRef] [Google Scholar]
- Histological and scanning electron microscope examination of root canal after preparation with Er: YAG laser microprobe: A preliminary in vitro study. J Clin Laser Med Surg. 2002;20:269-77.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of methodological variables on the push-out resistance to dislodgement of root filling materials: A meta-regression analysis. Int Endod J. 2016;49:836-49.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of root dentin conditioning protocols on the push-out bond strength of three calcium silicate sealers. Int J Adhes Adhes. 2015;60:104-8.
- [CrossRef] [Google Scholar]
- Effect of Nd: YAG and diode lasers on apical seal of root canals filled with AH plus and mineral trioxide aggregate-based sealers. J Dent (Tehran). 2018;15:30-40.
- [Google Scholar]
- Effect of Er: YAG laser on adhesion of root canal sealers. J Endod. 2002;28:185-7.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of effects on the adhesion of various root canal sealers after Er: YAG laser and irrigants are used on the dentin surface. J Endod. 2015;41:1331-6.
- [CrossRef] [PubMed] [Google Scholar]
- Sealing ability of a new polydimethylsiloxane-based root canal filling material. J Endod. 2008;34:204-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bioactivity of EndoSequence root repair material and bioaggregate. Int Endod J. 2012;45:1127-34.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of push-out bond strength of a new MTA-based sealer. Eur Arch Paediatr Dent. 2013;14:161-6.
- [CrossRef] [PubMed] [Google Scholar]
- Laboratory evaluation of the physicochemical properties of a new root canal sealer based on Copaifera multijuga oil-resin. Int Endod J. 2010;43:283-91.
- [CrossRef] [PubMed] [Google Scholar]
- Physical properties of MTA fillapex sealer. J Endod. 2013;39:915-8.
- [CrossRef] [PubMed] [Google Scholar]
- Leakage of five root canal sealers. Int Endod J. 1999;32:415-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antibacterial efficacy of AH Plus and AH26 sealers mixed with amoxicillin, triple antibiotic paste and nanosilver. J Dent Res Dent Clin Dent Prospects. 2016;10:220-5.
- [CrossRef] [PubMed] [Google Scholar]
- An in vitro evaluation of antimicrobial efficacy and flow characteristics for AH plus, MTA fillapex, CRCS and gutta flow 2 root canal sealer. J Clin Diagn Res. 2016;10:104-8.
- [CrossRef] [PubMed] [Google Scholar]