Translate this page into:
Current status of atraumatic restorative treatment in restorative dentistry

*Corresponding author: Sumit Sharma, Postgraduate, Department of Conservative Dentistry and Endodontics, Bangalore Institute of Dental Sciences and Hospital, Bengaluru, Karnataka, India. toothrocker2218@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma S, Raghu R, Shetty A. Current status of atraumatic restorative treatment in restorative dentistry. J Restor Dent Endod 2021;1(1):9-16.
Abstract
This review highlights the importance of atraumatic restorative treatment (ART) as a minimal intervention procedure for managing dental caries (pit and fissures caries) and restoring cavitated dentin carious lesions using restorative materials such as glass-ionomer cement. ART technique uses only hand instruments and requires no electricity. Its low cost and simplified protocol makes it more convenient and suitable for use in remote areas as well as underdeveloped nations with insufficient resources to provide the adequate restorative care. This technique can be used in all population groups including children, older people, and disabled. In the present scenario of the COVID-19 pandemic, the dental profession is facing a challenging task in managing restorative needs of the patients all over the world. ART technique is a safe and effective approach to manage the progression of carious lesions. As this technique involves no aerosol generation during the procedure, it should be well adopted in our routine practice by taking necessary precautions. The survival and retention rates of ART also appear to be fairly acceptable based on various studies.
Keywords
Atraumatic restorative treatment
Dental caries
Glass-ionomer cement
Cost-effectiveness
COVID-19
INTRODUCTION
Globally, dental caries has the highest prevalence amongst all oral diseases. It is estimated that 2.3 billion adults and over 530 million children are afflicted by dental caries.[1]
Despite advancements in preventive care, dental caries continues to pose a significant problem in most countries due to the increasing consumption of refined foods with high sugar content and inadequate exposure to fluoride. With increasing urbanization, the prevalence of dental caries continues to rise especially in the underprivileged sections of society.
Frencken proposed a simplistic yet minimally invasive approach to prevent dental caries. This technique is called atraumatic restorative treatment (ART) and consists of removing the carious tissue using hand instruments alone, without use of anesthesia followed by restoring the cavity with glass-ionomer cement (GIC). It was developed as a community-based oral health care program in the mid-1980s in Tanzania[2] and soon gained popularity worldwide.
Originally, ART was proposed for developing countries to benefit rural population, where resources were inadequate (poor accessibility to oral health-care units, electricity, etc.). In such conditions ART emerged as a predictable and successful technique as an early restorative simple care. Later, it was accepted in developed nations because of its “Atraumatic approach.”
DEFINITION AND ART CONCEPT
ART is defined as a minimally invasive approach in preventing dental caries and arresting its further progression.
It is recommended for sealing caries-prone pits and fissures and restoring cavitated dentine lesions using high-viscosity GIC.[3]
RATIONALE OF ART
Using a biological approach requires a minimal preparation of the cavity that retains sound tooth tissues and causes less damage to the teeth
Cost effective as compared to electric driven equipment
Need for local anesthesia is reduced
Less pain and psychological trauma
Accessible for all population groups.
GLASS IONOMER AS RESTORATIVE MATERIAL IN ART
ART is best performed using GIC. Fluoride releasing properties in GIC makes the tooth structure more resistant to dentinal caries. GIC that is specifically designed for ART is the high-viscosity materials (such as Ketac Molar Easymix®, GC Fuji IX, 3M ESPE, Seefeld, Germany).[4,5] They employ a high powder-to-liquid ratio, with improved mechanical properties, including wear resistance, compressive strength, and marginal adaptability.[4,5]
OTHER MATERIALS USED WITH ART
Resin composite, compomer, and resin-modified glass ionomer have also been used for restorations. However, autocured high-viscosity glass ionomer seems to be the most appropriate adhesive restorative material for use with ART.[6]
CLINICAL TRIALS
Various clinical trials have evaluated ART since its initial trial in 1986.[2,7]
INDICATIONS FOR USE
ART is used in situations where regular dental care is difficult due to lack of equipment or accessibility to a dental clinic
Performed only in small cavities that are accessible to hand instruments (involving the dentine)
Elderly and in truly debilitated patients
Patients with anxiety/nervousness
Public health programs
Both in primary and permanent teeth.
ART APPROACH AT PATIENT AND TOOTH LEVEL
At the patient level, one of the significant qualities of the ART approach is that it is all around acknowledged by patients because it infrequently requires a local anesthetic.
At the tooth level, depending on the current evidence from clinical shows that ART single-surface restorations using high viscosity GIC have a high rate of survival in both primary and permanent teeth. It has been suggested that ART restorations can be used for multiple-surface restorations in primary teeth; however, the survival rates are lower than those for single-surface restorations.[8]
| First pilot study | Tanzania | Excavators were used to remove soft, completely demineralized dentine from painful dentine cavities, followed by restoring with polycarboxylate cement | Results were presented in an international meeting, held at Tanzania in 1986 and a minimal intervention approach, called ART, was officially born[2] Inspired by the results, field study was instituted in Tanzania where polycarboxylate cement was replaced by medium viscous GIC |
| Early 1990s | Thailand (trial studies) | ART versus traditional amalgam approach[7] | The first set of ART criteria included wear of medium viscosity GIC and results showed low wear at the end of 3 year-trial which was later amended and is currently being used. |
| In 1992 | Thailand | Children treated with ART versus Traditional approach | Children who had been treated by ART were happily involved in the study, and those treated with the traditional rotary hand piece approach were unwillingly to participate |
| In 1994 | Thailand | Thailand study received regards from world pioneers embracing ART | ART approach was well appreciated by the World Health Organization on WHO day |
| In 1996 | Interim, ART examines had begun in Cambodia, Zimbabwe, and China | ART was being used in 25 countries | |
| In 1997 | FDI | A panel was setup to audit the new caries management reasoning of Minimal Intervention Dentistry | The report, depicting ART as one of the instances of MID, was published in 2000 in the International Dental Journal and was talked about at the 2002-FDI meeting held in Vienna. The General Assembly adopted ART as a minimal intervention approach[2] |
CONTRAINDICATIONS
Pulpal exposure
Signs of periapical involvement such as abscess and sinus tract
Lack of access to the cavity by hand instruments alone
There are clear signs of a cavity, for example, in a proximal surface but the cavity cannot be entered from the proximal or the occlusal directions.[9]
CLINICAL CONSIDERATIONS
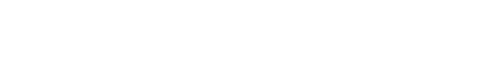
No special instruments are required to perform art under normal conditions as most of it can be found in regular dental clinics [Figure 1].
- A set of basic instruments and materials used for restorative procedures.
| Instruments required | Materials required |
|---|---|
| Mouth mirror | Cotton wool roll and pellet |
| Explorer | Glass-ionomer cement |
| Dental hatchet | Dentine conditioner |
| Spoon excavator | Petroleum jelly |
| Applier/carver | Wedge |
| Tweezers | Plastic strip |
| Mixing Pad and Spatula |
TECHNIQUE
Principal steps
The principal steps involved in ART are provided in the table below.
| Step 1: Before starting the procedure, make sure that all required ART armamentarium is arranged in orderly sequence to save number of steps. |
Step 2: Isolate the operating area using cotton rolls to prevent saliva or blood contamination which otherwise would interfere with GIC bond strength to tooth structure.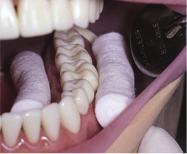
|
Step 3: Explore the cavity: First, carefully examine the operating site with mouth mirror and using dental explorer, remove any plaque or food debris from the pits and fissures if any without involving the deep penetration into the cavity. Second, clean the tooth surface by dampening the cotton followed by drying the surface using dry pellet.
|
Step 4: Widen the entrance of caries lesion: Necessary to follow this step in small carious lesion where opening of cavity is just minimal in order to remove the caries. Depending on the size of carious lesion (small or medium) a dental hatchet is used to gain access by stabilizing using finger rest, followed by placing the hatchet in the entrance of the cavity usually in the deepest part of the pit and the fissure. The tip of instrument is stabilized first and then moved backward and forward which breaks off the weak demineralized enamel, allowing enough access to the dentine caries.
|
Step 5: Excavation of caries: Hand excavators are used to remove soft infected dentin. Using the circular scooping motion of excavator is important to remove all the soft caries from the enamel-dentin junction (EDJ) before removing caries near the pulp. Removing soft caries leave the unsupported enamel with dentin at EDJ. This unsupported enamel breaks off very easily and should therefore be removed using the blade of enamel hatchet. Repeat this process until all the thin unsupported enamel has been removed and no caries is left behind.
|
Step 6: Conditioning of the prepared cavity: To improve the chemical and mechanical bonding of the GIC to the tooth structure, the cavity walls must be clean. The smear layer should be removed using a chemical solvent. A dentin conditioner containing 10–40% solution of polyacrylic and its copolymers is especially used for the same. Dip a cotton pellet in the conditioner and then clean the entire cavity for 10–15 s.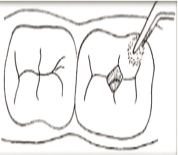
|
Step7: Mix glass ionomer: To have excellent results, ensure a good consistency mix and follow the manufacturer’s instructions. The correct powder to liquid ratio must be maintained while mixing.
|
| Step 8: Restoring the cavity: After mixing GIC, it must be immediately inserted into the cavity in small amounts using the carver to prevent incorporation of air bubbles. Make sure the mixture goes around the margins of the cavity especially under the overhanging enamel. Place a little extra material on adjacent pits and fissures. Rub a small amount of petroleum jelly on the gloved index finger and restore the cavity with gentle press using finger. This is known as “the press-finger technique.” Remove the excess material without dislodging the restoration. 
|
| Step 9: Check the bite: Place an articulating paper on the restored tooth, check for high points and remove any excess cement if needed. Advise the patient not to eat for at least the following 1 h. 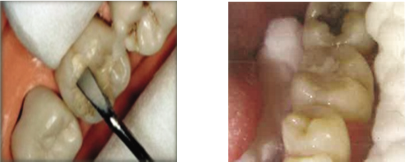
|
TECHNIQUE FOR RESTORING MULTIPLE-SURFACE CAVITIES
Isolate the working area
Ensure that the cavity is free of caries
Place matrix strip around the teeth followed by inserting a wedge below the interproximal contact area to keep the strip in stabilized position
Follow the same procedure of conditioning as described to clean in one surface cavity preparation
Mix the GIC is to fill the cavity, to ensure it is slightly overfilled
Grasp the matrix strip firmly with index finger and thumb. Remove the wedge and strip once the restorative material sets and apply petroleum jelly on it
Remove any excess filling if present; check the height of the filling with articulating paper.
SUCCESS RATE OF ART RESTORATION
Since the beginning, researchers were interested in the length of survival of ART restorations (Phantumvanit et al., 1996; Frencken et al., 1998).[10]
In a study conducted in Kenya, 804 children, aged 6–8, overall survival was 44.8% after 1 year. Survival rate was highest with restorations of size between 2 and 3 mm.[11]
Over a period of 3 years study in Zimbabwe by Frencken et al., found that experienced operators placed better, longer lasting ART restorations than inexperienced ones. One-surface survival rates were 88.3%.[12]
In a clinical field trial by Mallow et al., in a high school in rural Cambodia on 53 students aged between 12 and 17 years with dental caries, it was found that after 1 year, 76.3% of restorations were successful and 57.9% were still successful at 3 years.[13]
In Mexico, 118 children aged 5–18 years were given restorations using ART. After 2 years, 66% of restorations were retained.[14]
Lo et al. reported a 6-year follow-up of ART in school going children in China, concluded that cumulative survival rates of the small restorations remained high throughout the study, being above 90% over the first 3 years and 85% up to 6 years.[15]
In a 2-year follow-up, 89•6% of all ART restorations were considered successful.[16]
A meta-analysis, in 2006, which addressed the success rates of ART in primary and permanent dentitions, concluded high mean survival rates for single-surface ART restorations using high viscosity GICs.[17]
In overview, ART survival and retention rate appears to be acceptable and because of its minimal invasive nature, it can be routinely followed in dental practice and can be used in both primary and permanent dentition involving single surface restorations of posteriors compared to multi-surface restorations.
ART AND SECONDARY CARIES
The expected high percentage of restoration failures due to the development of so-called secondary caries was one of the concerns expressed in the early years of ART development because a layer of soft carious dentin is sometimes left behind in the cavity after ART caries excavation. However, secondary caries at the margins of ART glass-ionomer restorations was reported to be low. This finding is supported by the results of a systematic review which showed that glass ionomer had a higher caries-preventive effect than amalgam restorations in permanent teeth, with no difference in primary teeth.[18]
COST OF ART
ART approach is considered to be economic and costs less than conventional treatments. A study conducted by Mickenautsch et al., compared the cost of ART and conventional treatment found that the ART approach was cost-effective. The capital cost of ART was 50% less when performing ART, quality of glass-ionomer should not be compromised as low quality of glass ionomer can lead to ineffective results and should not be considered for ART.[19]
COMPARISON OF ART RESTORATIONS VERSUS TRADITIONAL RESTORATIONS
In a meta-analysis based on five randomized clinical trials in which ART restorations using glass ionomer were compared with amalgam restorations by Frencken et al. concluded that there appeared to be no difference in survival rates between single-surface ART restorations using glass ionomer and amalgam restorations in permanent teeth over the first 3 years.[9] One systemic review by Dorri et al., combined the studies which got published between 2002 and 2016 comprising a total 15 eligible studies, concluded that low-quality evidence suggests that ART using H-GIC may have a higher risk of restoration failure than conventional treatment for caries lesions in primary teeth. Although, many studies evaluated the effects of ART on the primary dentition, yet further studies are needed to have a broader view on the same.[20]
ART IN DISABLED PATIENTS
Children who are mentally/physically challenged face numerous difficulties to dental treatment.[21]
Disabled patients may present difficulty in managing with traditional treatment methods performed in the dental chair.[22]
A study conducted by Molina et al., to assess the 3-year cumulative survival rate of ART in disabled patients concluded that survival rates after 3 years of ART restoration were satisfactory. They concluded that this is an effective method to treat carious lesions in disabled.[23]
ART IN OLDER PEOPLE
A study conducted among elderly patients revealed that 79% of the ART restorations placed were considered successful after 1 year ART was well appreciated by the homebound elderly.[24] Thus, ART can be seen as an effective approach in dental healthcare for elderly. Another study was carried out for treating root caries in older people with a mean age of 78.6 years in comparison to that of traditional treatment using a resin-modified glass ionomer. The survival rates for ART were 87.0% and 91.7% for conventional treatment after 1 year.[25] In regards to the global growth in elderly people over the coming decades, serious attention should be given to the impact of the ART approach as part of their oral care.
LIMITATIONS OF ART
| 1. Technique is confined to single-surface restorations |
| 2. ART approach cannot be performed in areas of limited accessibility |
| 3. Manual manipulation of glass-ionomer cement can lead to improper mix (W/P ratio) resulting in weaker restorations |
| 4. Use of hand instruments for longer period might cause hand fatigue of operator |
| 5. ART technique being quite simple is a delusion, in fact every step should be done carefully with proper technique |
MODIFICATIONS IN ART
Modifications to true ART, is generally carried out in places where traditional dental equipment has been generally available unlike in field situations.
This modified approach is generally done with the use of rotary instrument (drill to open the tooth cavity) followed by “Original ART” procedure including cleaning and restoring the cavity. The use of rotary equipment was advised to make the whole procedure faster and easier.[26]
Nevertheless, this is a debatable matter as opening the cavity with rotary instruments followed by cleaning and restoring with adhesive material cannot be justified saying it as modified ART.[27]
ART AS FRONTLINE CHOICE AMONG CLINICIANS IN COVID-19 CRISIS? WHY NOT
Recently COVID-19, also known as coronavirus disease, first emerged in China and has spread worldwide. It has devastated the entire globe and is a matter of grave concern. The World Health Organization has declared coronavirus disease outbreak a pandemic on March 11, 2020.[28] COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 infection.
Several dental care centers in affected nations have been completely closed or have been providing minimal treatment for emergency cases. This could be due to the unavailability of a universal protocol or guidelines governing dental care in a pandemic. Dentists who conduct aerosol generating procedures may unknowingly get directly exposed to patients who have been infected but not yet diagnosed COVID-19 patients. Inhalation of airborne particles and aerosols generated during procedure can be a high-risk factor to which dentist and auxiliaries are directly exposed. Hence, dentists need to concentrate on preventive strategies to avoid the spread of COVID-19.
These preventive strategies can be in the form of personal protective equipment (including masks, gloves, gowns, and goggles or face shields) or in the form of minimally invasive approach. Since ART involves no aerosols generation and is performed with hand instruments it is a precautionary measure for both the dentist and the patient. Therefore, ART can be suggested as a preventive measure and minimal intervention during COVID-19 crisis.
It is well said “Prevention is better than cure.”
CONCLUSION
ART technique has proven to be a successful approach due to its minimal invasive nature. It is a fusion of preventive and curative care which should be combined along with appropriate dietary modifications, good oral hygiene, and use of fluoride toothpaste to minimize the occurrence of caries lesions.
ART has a great potential to eliminate aerosol generation. Therefore, in the current scenario, it is highly advantageous to incorporate ART into routine clinical practice adhering to proper guidelines.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789-8583.
- [CrossRef] [Google Scholar]
- Evolution of the ART approach: Highlights and achievements. J Appl Oral Sci. 2009;17:78-83.
- [CrossRef] [PubMed] [Google Scholar]
- Atraumatic restorative treatment and glass-ionomer sealants in a school oral health programme in Zimbabwe: Evaluation after 1 year. Caries Res. 1996;30:428-33.
- [CrossRef] [PubMed] [Google Scholar]
- Atraumatic restorative treatment (ART): A three-year community field trial in Thailand--survival of one-surface restorations in the permanent dentition. J Public Health Dent. 1996;56:141-5.
- [CrossRef] [PubMed] [Google Scholar]
- Twenty-five-year atraumatic restorative treatment (ART) approach: A comprehensive overview. Clin Oral Investig. 2012;16:1337-46.
- [CrossRef] [PubMed] [Google Scholar]
- An atraumatic restorative treatment (ART) technique: Evaluation after one year. Int Dent J. 1994;44:460-4.
- [Google Scholar]
- Minimal intervention dentistry: Part 5. Atraumatic restorative treatment (ART)-a minimum intervention and minimally invasive approach for the management of dental caries. Br Dent J. 2013;214:11-8.
- [CrossRef] [PubMed] [Google Scholar]
- Essentials of Public Health Dentistry (5th ed). New Delhi: Arya Medi Publishing; 2017.
- [Google Scholar]
- Effectiveness of single-surface ART restorations in the permanent dentition: A meta-analysis. J Dent Res. 2004;83:120-3.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of the cavity-size on the survival rate of proximal ART restorations in primary molars. Int J Paediatr Dent. 2009;19:423-30.
- [CrossRef] [PubMed] [Google Scholar]
- Three-year survival of one-surface ART restorations and glass-ionomer sealants in a school oral health programme in Zimbabwe. Caries Res. 1998;32:119-26.
- [CrossRef] [PubMed] [Google Scholar]
- Restoration of permanent teeth in young rural children in Cambodia using the atraumatic restorative treatment (ART) technique and Fuji II glass ionomer cement. Int J Paediatr Dent. 1998;8:35-40.
- [CrossRef] [PubMed] [Google Scholar]
- Atraumatic restorative treatment for prevention and treatment of caries in an underserved community. Am J Public Health. 2005;95:1338-9.
- [CrossRef] [PubMed] [Google Scholar]
- Six-year follow up of atraumatic restorative treatment restorations placed in Chinese school children. Community Dent Oral Epidemiol. 2007;35:387-92.
- [CrossRef] [PubMed] [Google Scholar]
- The atraumatic restorative treatment (ART) approach to restoring primary teeth in a standard dental clinic. Int J Paediatr Dent. 2003;13:172-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Atraumatic Restorative Treatment (ART) approach for managing dental caries: A meta-analysis. Int Dent J. 2006;56:345-51.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative cost of ART and conventional treatment within a dental school clinic. SADJ. 2002;57:52-8.
- [Google Scholar]
- Low-cost GICs reduce survival rate in occlusal ART restorations in primary molars after one year: A RCT. J Dent. 2017;57:45-50.
- [CrossRef] [PubMed] [Google Scholar]
- Atraumatic restorative treatment versus conventional restorative treatment for managing dental caries. Cochrane Database Syst Rev. 2017;12:CD008072.
- [CrossRef] [PubMed] [Google Scholar]
- Access barriers to dental health care in children with disability. A questionnaire study of parents. J Appl Res Int Disabil. 2015;29:139-45.
- [CrossRef] [PubMed] [Google Scholar]
- Three-year survival of ART high-viscosity glass-ionomer and resin composite restorations in people with disability. Clin Oral Investig. 2017;22:461-7.
- [CrossRef] [PubMed] [Google Scholar]
- Atraumatic dental treatment among Finnish elderly persons. J Oral Rehabil. 2002;29:435-40.
- [CrossRef] [PubMed] [Google Scholar]
- ART for treating root caries in older people. Evid Based Dent. 2007;8:51.
- [CrossRef] [PubMed] [Google Scholar]
- UK dentists attitudes and behavior towards atraumatic restorative treatment for primary teeth. Br Dent J. 2005;199:365-9.
- [CrossRef] [PubMed] [Google Scholar]
- The correct use of the ART approach. J Appl Oral Sci. 2010;18:1-4.
- [CrossRef] [PubMed] [Google Scholar]
- WHO Virtual Press Conference on COVID-19 In: World Health. Organization. 2020a. Available from: https://www.who.int/docs/defaultsource/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf [Last accessed on 2020 Mar 29]
- [Google Scholar]